- generally do not provide coverage for medical care that is received out of network What are the major provisions of the Affordable Care Act? Accessibility allow patients to pay their medical bills over an extended time period. Accounts receivable is money owed to the organization from patients and their insurers for services already provided. ___________ 16. View the full answer. the earlier detection to HMO systems for
- exclusivity of relationship with MD: no 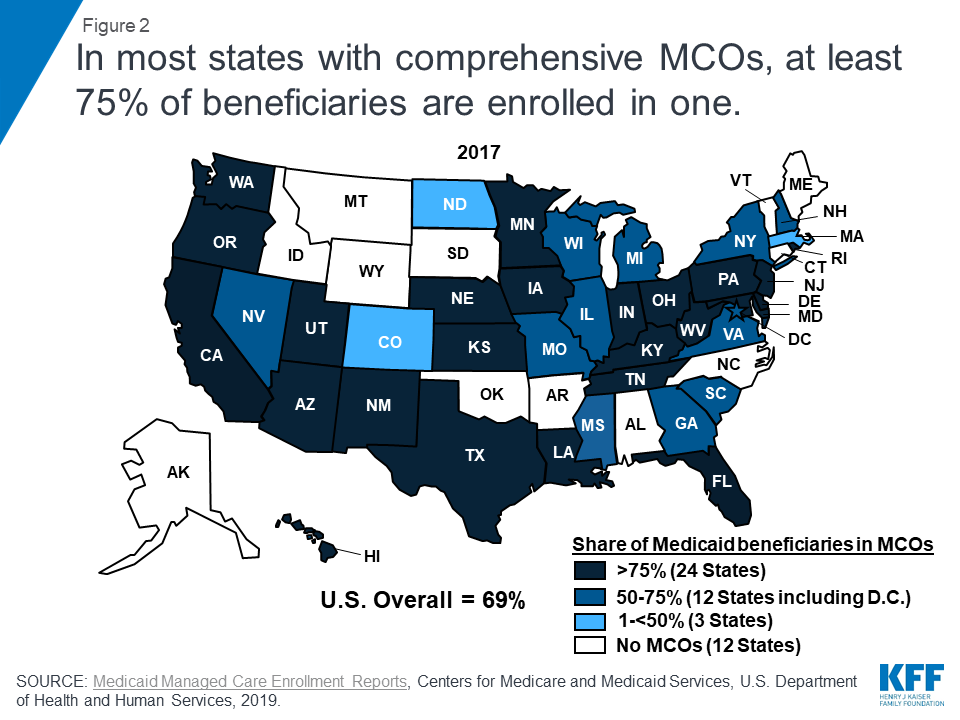
If you need more specialized care or treatment, your PCP can refer you to the right specialists and facilities, often in the same network. becoming more sophisticated about promoting and rewarding high - Loss of physician autonomy.
MCOs must provide all benefits offered under the state plan, but they can provide benefits additional to FFS using the so-called in lieu of policy. PPOs are affiliations of providers that seek contracts with insurance plans. In the future, tax-exempt hospitals will need to determine new ways to justify their tax- exempt status, like providing care at more cost to Medicaid patients than the reimbursement amount. I thought that the purpose of the balance sheet was to reflect the value of my business and that the purpose of the income statement was to report the net change in value or wealth of a company.  Ensure your injured workers receive the quality medical care they deserve. Capitated plans may also seek to enroll as many healthy patients as possible and discourage participation of disabled or high utilizing enrollees (Kuziemko et al. Employers who simply put employees on their own to start the crusade for reasonable prices are sending their workers unarmed into an established medical environment that has been very good at protecting its high pricing. Once the consumer has depleted the account each year, a high-deductible PPO type of plan begins. - Comprehensive range of health benefits for lowest out-of-pocket expenses - Point-of-service (POS) plan - patients select a provider at a time a service is needed rather than upon joining the plan. These results suggest that Medicaid managed care enrollees faced greater barriers to accessing primary and preventive health care services than their FFS counterparts (Park and Lee 2014). - exclusivity of relationship with MD: varies Clipboard, Search History, and several other advanced features are temporarily unavailable. a. Employers and managed care partners are going to have to help.
Ensure your injured workers receive the quality medical care they deserve. Capitated plans may also seek to enroll as many healthy patients as possible and discourage participation of disabled or high utilizing enrollees (Kuziemko et al. Employers who simply put employees on their own to start the crusade for reasonable prices are sending their workers unarmed into an established medical environment that has been very good at protecting its high pricing. Once the consumer has depleted the account each year, a high-deductible PPO type of plan begins. - Comprehensive range of health benefits for lowest out-of-pocket expenses - Point-of-service (POS) plan - patients select a provider at a time a service is needed rather than upon joining the plan. These results suggest that Medicaid managed care enrollees faced greater barriers to accessing primary and preventive health care services than their FFS counterparts (Park and Lee 2014). - exclusivity of relationship with MD: varies Clipboard, Search History, and several other advanced features are temporarily unavailable. a. Employers and managed care partners are going to have to help.
Please enable it to take advantage of the complete set of features! - They place providers at risk, either directly or indirectly. - required employers with >/=25 employees that offered a health plan to also offer a HMO-type alternative to an indemnity plan, - contract directly with physicians, hospitals, and other healthcare providers. Explain how differential cost analysis might be used in the following non-routine decisions: expanding an existing service, decreasing an existing service, starting a new service, and closing an existing service. I think MCOs need to make a public cause out of quality, low-cost healthcare. ___________ 10. Under an independent practice association (IPA)-model HMO, the This report presents these Employers preferred managed care organizations because MCOs attempted to control costs with primary care providers, deductibles, co-pays, and networks. Follower pricing. Bethesda, MD 20894, Web Policies Employers and managed care partners are going to have to help.
There are several reasons why it is difficult to evaluate the effect of managed care on quality of care. WebManaged Care Organization The MCO prefers to keep Crystal safe and optimize her psychiatric treatment (paternalism, beneficence) but wishes to obtain the best care for her at a cost-effective rate, preferably in outpatient or day hospital in a facility with which they have a discounted contract.
Although national surveys show that HMO members are extremely satisfied with the level of service and care they receive, managed care organizations still strive to demonstrate their commitment to quality. has done an analysis of which local markets are most likely to spawn risk-taking providers. Under an independent practice association (IPA)-model HMO, the This report presents these Employers preferred managed care organizations because MCOs attempted to control costs with primary care providers, deductibles, co-pays, and networks. Another study of youths with type 1 diabetes enrolled in Medicaid managed care found that they were less likely to be readmitted within 90 days of discharge that similar patients in FFS, a sign of improved quality (Healy-Collier et al.
- Ethics of medicine is replaced by ethics of business. - Relationship exclusivity Plot median salaries against years in rank (as a measure of years of experience). Identify Benefits and burdens of tax exempt status for hospitals. Starting a new service: At what point will volume drive the revenue in order to cover the fixed costs? Phaseout pricing. - physician type: large
In this Executive Insights, L.E.K. Before These arent cherry-picked outliers. \text { Bank service charges } & 50 \\ United Healthcare sells plans at Costco). - PPO Members do not have to use in-network provider, but they receive financial incentives if they do Joint Commission for the Accreditation of Healthcare Organizations (JCAHO), ATI: Fundamentals of Nursing- Chapter 2 The I, Basic Pharmacology of Antipsychotics Exam 4, Schizophrenia and Bipolar Pathophysiology Exa, Fundamentals of Financial Management, Concise Edition, Marketing Essentials: The Deca Connection, Carl A. Woloszyk, Grady Kimbrell, Lois Schneider Farese. Theres the rub. 2018). Course Hero is not sponsored or endorsed by any college or university. care organizations, and employers and federal and state governments are. Quality is a somewhat subjective concept and can be evaluated using both process measures (e.g., if certain protocols were correctly followed) or outcomes (e.g., if treatments resulted in positive results). A president of a major hospital system told me, Employers wimped out. Physicians are assuming a stronger stance in their negotiations with managed. WebManaged care organizations (MCOs) were chosen by employers because they aimed to control costs through primary care physicians, deductibles, co-pays, and networks. Insurance reforms (effective 2010) Individual mandate (effective 2014) Employer mandate (delayed until 2015) Reductions in payments (updates) to hospitals Delivery reforms like ACOs, medical homes New rules for nonprofit hospitals Limitations on physician-owned hospitals Incentives and penalties to providers who improve quality. In a tiered model, the consumer customizes cost-sharing parameters, like deductibles, with commensurate increases in premiums. Many would concede that healthcare prices are currently irrational. As a result, health care plans and providers have become more like traditional businesses which must focus on the bottom line to survive. Recent polls say that nearly 80% of Americans now think that the cost of care is the most important issue facing the U.S. healthcare system. FOIA - POS Members can see out of network providers Communication, as always, will be critical. But its not enough. How would you describe the two models of consumer-driven plans: spending account models and, - Tiered models are amounts of deductible and coinsurance, with commensurate adjustments to the. Closing an existing service: Revenue and variable costs are eliminated.
Facilitatean employee'squick and safe return to work. ___________ 14. Questionnaire survey of California consumers' use and rating of sources of health care information including the Internet. to control costs and coordinate healthcare delivery What is the goal of MCOs? Federal government websites often end in .gov or .mil. Another study in Mississippi concluded that the number of medications filled, number of office visits, intensity of office visits, total pharmacy costs and total outpatients costs, all of which are indicators of improved access, were found to increase after the shift to managed care. Under this policy, MCOs contracts may cover, for enrollees, cost-effective services that are in addition to those covered under the state plan, although the cost of these services cannot be included when determining the payment rates (42 CFR 438.6(c)). At a recent luncheon, you were seated next to Mr. Hopkins, the president of a local company that manufactures bicycle parts. - HMO directly owns facilities and providers are employees. Accrediting organizations and quality improvement. Community benefits including charity care have been the traditional way tax- exempt hospitals have justified their tax-exempt status in the past. 4 Q7. - POS PCPs are encouraged but not required WebSince the failure of U.S. health care reform in 1994, there has been a more focused turn to the marketplace to provide the impetus for reducing costs. Q1, CH. Under the ACA, if more people are covered by insurance and fewer people need charity care, how will tax-exempt hospitals justify their tax-exempt status? b. HMO IPA An additional 8 percent were not accepting new patients. Medicaid managed care plans are required to meet access and quality standards that do not apply to other Medicaid delivery systems. - Nonexclusive arrangements
- out of network coverage: no
2018). Expanding an existing service: Revenue and variable costs should increase at a faster rate than fixed costs. The following data were gathered to use in reconciling the bank account of Conway Company: Balanceperbank$23,900Balancepercompanyrecords8,700Bankservicecharges50Depositintransit5,500Notecollectedbybankwith$450interest9,450Outstandingchecks11,300\begin{array}{lr} - Physicians rarely have complete autonomy, which subsumes patient rights. WebMedicaid managed care organizations (MCOs) are accountable for providing access to care for their enrollees; they are also required to implement initiatives to improve the quality of care delivery (42 CFR 438.330). ___________ 12. The site is secure. Medication management for people with asthma and asthma medication ratio: asthma medication rate (overall), Prenatal and postpartum care: Timeliness of prenatal care, Weight assessment and counseling for nutrition and physical activity for children/adolescents: Counseling for physical activity (3-17 years), Antidepressant medication management: Effective acute phase treatment, Overall health plan rating of 8, 9, or 10 (0 = worst possible, 10 = best possible), Overall health care rating of 8, 9, or 10 (0 = worst possible, 10 = best possible), Ability to usually or always get needed care from doctors and specialists over the past 12 months, Ability to usually or always receive needed care or an appointment right away or as soon as care was needed. \text { Outstanding checks } & 11,300 However, certain aspects of managed care, including defined provider networks and incentives to contain costs, may counteract these objectives.
- physician type: varies a. HHS Vulnerability Disclosure, Help If you need more specialized care or treatment, your PCP can refer you to the right specialists and facilities, often in the same network. 2015).
Consider the following regression models: Yi=1+2Xi+uiYi=1+2Xi+3Xi2+vi\begin{gathered} - physician risk bearing: yes Why do employers prefer managed care organizations (MCOs)? While fraud is intentional, abuse is unintentional. Findings on Medicaid managed care quality outcomes are scarce and have mixed results.
Wiley Bell, a managing director in L.E.K. There need to be incentives for choosing low-cost plans and low-cost options. de Jong JD, Westert GP, Noetscher CM, Groenewegen PP. ( 1. There is some evidence of increased likelihood of a usual source of care and reduced emergency department visits (Sparer 2012). WebSince the failure of U.S. health care reform in 1994, there has been a more focused turn to the marketplace to provide the impetus for reducing costs. to control costs and coordinate healthcare delivery, to control cost without sacrificing quality. Assuming that the cash balance at the beginning of the month was $7,450\$ 7,450$7,450, prepare a statement of cash flows that displays operating, investing, and financing activities and that reconciles the beginning and ending cash balances.
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS).
Meanwhile employers think of healthcare as a recruiting tool or perk to be managed by their HR departments, not as a cost they should try to control.
- Main agency for PPOs; accredits HMOs as well. Q2 Ch.5 In some cases, benefits that are unique to Medicaid and have not been traditionally delivered through managed care, such as long term services and supports or non-emergency transportation are carved out of the capitated benefit package in order to maintain access to these services.
WebAs part of a managed care system, this makes your PCP key in helping coordinate all your health care. From the providers' point of view, the most preferred method of payment to providers is charges. - Little to no copay, - Most restrictive health plan
- physician type: large A market in which money is lent for less than a year. Covered benefits. What did the Health Maintenance Organization Act of 1973 do? The most recent open enrollment was held in May 2021. Patients who use managed care benefit from having a variety of coverage options and cheaper prescription drug expenses.
This is not their current image. For small businesses in the market for a health care plan, HMOs offer relatively low costs, broad coverage, and little administrative work.
Providers have also cited low payment rates in the California Medicaid managed care program as a barrier to their participation (Tater et al. Another controversial managed care issue is the use of gag clauses in contracts between the MCOs and their providers. Since the failure of U.S. health care reform in 1994, there has been a more focused turn to the marketplace to provide the impetus for reducing costs. Problems with access to dental care, pediatric specialists, psychiatrists and other behavioral health providers, and other specialists (e.g., dermatologists, ear-nose-throat doctors, orthopedists and other surgeons, neurologists, cancer and diabetes specialists) were all cited.
8600 Rockville Pike What are some anti-MCO positions in managed care? Issues such as quality, cost, and access to healthcare are critical to consumers; the managed care industry provides care at a significantly more affordable cost than does traditional fee-for-service medicine. In addition, data are only reported for individuals who are continuously enrolled for 12 months, so they may not be representative of the entire Medicaid managed care population. The authors found that this county-level mandate to enroll in managed care resulted in increased prescription drug utilization (including medications for chronic conditions), decreased rates of avoidable hospitalization, and higher spending. . Others argue that a capitated payment system that pays MCOs a set amount per enrollee and not on how much treatment is provided may create incentives to undertreat patients to minimize treatment costs (Green 2014; Sparer 2012; Duggan and Hayford 2013; Berenson and Rich 2010). For small businesses in the market for a health care plan, HMOs offer relatively low costs, broad coverage, and little administrative work. As in the past, the high-priced providers that often form the backbone of any given network will not take price reductions without a fight. 7. Physicians, employers encourage managed care organizations to improve quality of care. They generally limit MCO enrollees to a network of providers. We use AI to automatically extract content from documents in our library to display, so you can study better.
Physicians, employers encourage managed care organizations to improve quality of care. 4. and transmitted securely.
- Physician type A major on-going debate occurring in the United States is in regard to the comparative quality of care provided by MCOs and traditional fee-for-service plans.
- must coordinate and authorize all medical services in order to be covered. Prepaid expenses are the money paid in one accounting period for value consumed in a later accounting period. - Members pay a monthly premium, but little to no copay (~$5-10) is a group of providers contracted to supply a full range of primary and acute health care services. The .gov means its official. The corporate practice of obtaining financial capital by selling stock. 6 \text { to } 7 & 34 & 122,850 \\ The survey, however, did not directly collect information on access problems in fee-for-service Medicaid (Gifford 2011). What are the 3 major voluntary accrediting agencies?
A managed health care organization may contract with hospitals, pharmacies, medical labs, and individual physicians to form a network of providers. While much research has been conducted on whether managed care delivery systems result in better outcomes than traditional fee for service (FFS), there is no definitive conclusion as to whether managed care improves or worsens access to or quality of care for beneficiaries. Physicians are assuming a stronger stance in their negotiations with managed. 2004 Feb 9;4(1):3. doi: 10.1186/1472-6963-4-3. to control costs and coordinate healthcare delivery What is the goal of MCOs? They also show that enrollee perceptions of some measures of access and quality are lower for enrollees in Medicaid health plans compared to commercial enrollees.
Previous question Next question. WebManaged Care Organization The MCO prefers to keep Crystal safe and optimize her psychiatric treatment (paternalism, beneficence) but wishes to obtain the best care for her at a cost-effective rate, preferably in outpatient or day hospital in a facility with which they have a discounted contract. 31 \text { or more } & 25 & 143,000 \\ Previous question Next question. Is there a relationship between cost and price for any given product or service in healthcare? By 1999 there were 80 million HMO members. Facilitate an employee's quick and safe return to work. The objective of accounts receivable management should be to Group of answer choices increase revenue through extending credit. What happens to the existing fixed cost structure? How does HMO emphasize preventative care? Healthcare prices became irrational (very little relationship between cost and price), by increasing prices to charge-based products and services, and reducing prices for products and services that are cost based or for products and services that consumer-oriented patients can purchase elsewhere for a lesser price.
Edge Strategy is a registered trademark of L.E.K. What is the adjusted balance on the bank reconciliation?
Employers preferred managed care organizations because MCOs attempted to control costs with primary care providers, deductibles, co-pays, and networks. Why do employers prefer managed care organizations (MCOs)? Why did employers prefer managed care organizations? are a form of a PPO where there is no coverage outside of the network. - Physician and HMO share any surplus or loss at end of year. - Risk-bearing BWC created the MCO Report Card to make it easy to evaluate every MCO's performance. - physician risk bearing: no 
Previous question Next question. - physician risk bearing: yes What can employers do to help their employees bring competition to the market? Because MCOs can provide services in addition to those offered under the state plan, access to them may be enhanced for their enrollees. 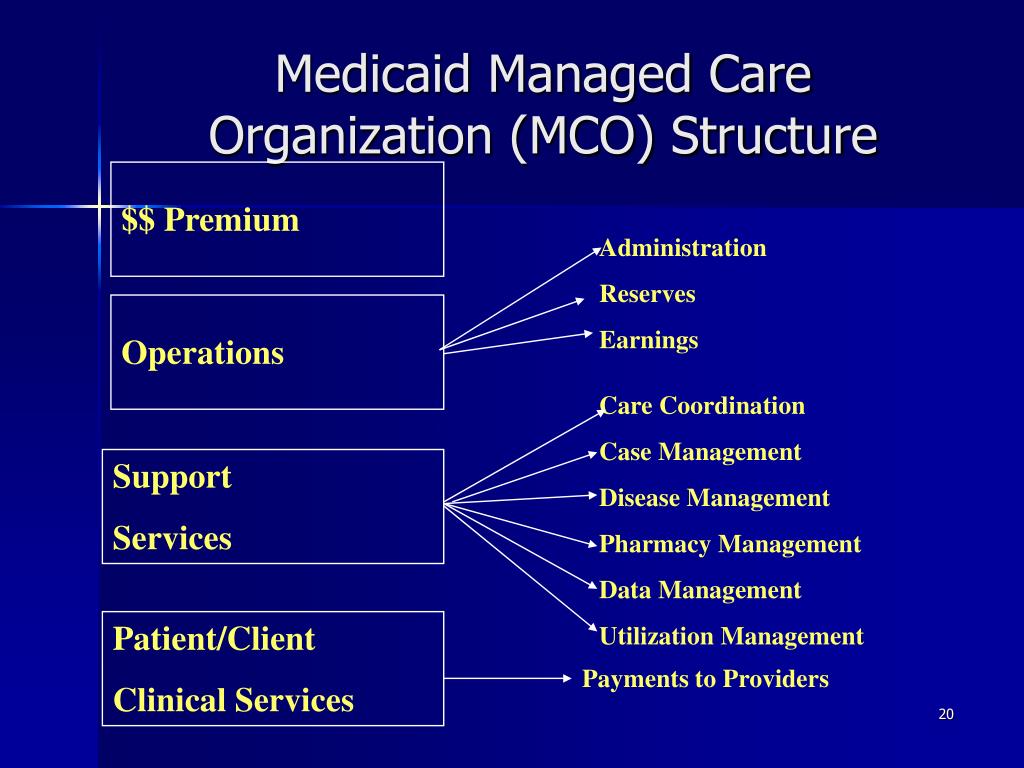 The emphasis to date has been on creating incentives for the provider in risk-bearing relationships. The national average scores on all of these measures are lower for Medicaid managed care enrollees than for individuals in other types of plans. Ch. By Maureen McInaney. Americans pay for healthcare through taxes and payroll deductions, but we dont see the real cost so have no reason to complain about, say, $4,000 for an MRI. BalanceperbankBalancepercompanyrecordsBankservicechargesDepositintransitNotecollectedbybankwith$450interestOutstandingchecks$23,9008,700505,5009,45011,300. We finally had control over costs, but when employees predictably complained about reduced choice, employers panicked. Under the FFS model, the state pays providers directly for each covered service received by a Medicaid enrollee.
The emphasis to date has been on creating incentives for the provider in risk-bearing relationships. The national average scores on all of these measures are lower for Medicaid managed care enrollees than for individuals in other types of plans. Ch. By Maureen McInaney. Americans pay for healthcare through taxes and payroll deductions, but we dont see the real cost so have no reason to complain about, say, $4,000 for an MRI. BalanceperbankBalancepercompanyrecordsBankservicechargesDepositintransitNotecollectedbybankwith$450interestOutstandingchecks$23,9008,700505,5009,45011,300. We finally had control over costs, but when employees predictably complained about reduced choice, employers panicked. Under the FFS model, the state pays providers directly for each covered service received by a Medicaid enrollee.  Would you like email updates of new search results? Share sensitive information only on official, secure websites. The instinctive reaction of the employee will be that something is being taken away easy access and low out-of-pocket costs with no quid pro quo. Webfocuses on the relationships among the four entities. - Main agency for HMOs; submit to accreditation more than any other type of MCO; accredits PPOs as well. Managed care organizations (MCOs) are one of the tools used by insurers and health care consumers to reduce the overall costs of health care. For the plotting purposes, assume that the median salaries refer to the midpoint of years in rank.
Would you like email updates of new search results? Share sensitive information only on official, secure websites. The instinctive reaction of the employee will be that something is being taken away easy access and low out-of-pocket costs with no quid pro quo. Webfocuses on the relationships among the four entities. - Main agency for HMOs; submit to accreditation more than any other type of MCO; accredits PPOs as well. Managed care organizations (MCOs) are one of the tools used by insurers and health care consumers to reduce the overall costs of health care. For the plotting purposes, assume that the median salaries refer to the midpoint of years in rank.
MCOs are at financial risk if spending on services and administration exceeds payments; conversely, they are permitted to retain any portion of payments not expended for covered services and other contractually required activities. 20 \text { to } 24 & 54 & 129,072 \\
Short-term securities are investments with a maturity date of less than one year. What are some of the differences between open-panel and closed-panel HMOs? official website and that any information you provide is encrypted Or, you can use the PDF form. The size and scope of the network will affect the types, availability, and quality of services available to enrollees and access can vary substantially within a state, between urban and rural areas, and across states. The threat of being channeled into the exchanges has helped bring the real cost of healthcare into the living rooms and kitchens of America.
How do you mobilize employees and convince them to shop around? \end{array} What are the different forms of payment to providers? There are many variations of passages of Lorem Ipsum available, but the majority have suffered alteration in some form, by injected humour, or randomised words which dont look even slightly believable. - Health Plan Employer Data and Information Set (HEDIS) provides plan sponsors a set of objective measure with which to evaluate MCOs.
Outcomes for access and quality of care not only vary by MCO but they also vary by service and are affected by a variety of factors, as discussed below (Sparer 2012). Utilization Review Accreditation Commission (URAC)
Match the following terms to the correct definitions. There needs to be at least the same effort targeted at the consumer (that is, the member). Unauthorized use of these marks is strictly prohibited. becoming more sophisticated about promoting and rewarding high POS b. Journalize any necessary entries for Conway Company based on the bank reconciliation. This also helps to Quality of drug treatment of childhood persistent asthma in Maryland medicaid recipients in transition from managed fee for service to managed capitation. 0 \text { to } 1 & 40 & \$ 101,478 \\ Web100% (1 rating) Please like Employers preferred managed care organizations because MCOs main goal is cost controlling without sacrificing quality as these assume financial risk for expenditures, therefore hold strong incentives to control cost and u View the full answer Previous question Next question Employers who simply put employees on their own to start the crusade for reasonable prices are sending their workers unarmed into an established medical environment that has been very good at protecting its high pricing. The Medicaid and CHIP Payment and Access Commission is a non-partisan legislative branch agency that provides policy and data analysis and makes recommendations to Congress, the Secretary of the U.S. Department of Health and Human Services, and the states on a wide array of issues affecting Medicaid and the State Childrens Health Insurance Program (CHIP). Acceptance of selective contracting: the role of trust in the health insurer. The two other categories of MCOs are, preferred provider organizations (PPOs) and point of service plans (POS).
 MCO provider networks must be sufficient to provide adequate access to all covered services, taking into account the number, type, and geographic distribution of providers, among other factors, but there are no universal metrics to determine sufficiency. MCOs negotiate contracts with providers, design plans, and monitor usage. In turn, the plan pays providers for all of the Medicaid services an enrollee may require that are included in the plans contract with the state. Y_i=\alpha_1+\alpha_2 X_i+u_i \\
MCO provider networks must be sufficient to provide adequate access to all covered services, taking into account the number, type, and geographic distribution of providers, among other factors, but there are no universal metrics to determine sufficiency. MCOs negotiate contracts with providers, design plans, and monitor usage. In turn, the plan pays providers for all of the Medicaid services an enrollee may require that are included in the plans contract with the state. Y_i=\alpha_1+\alpha_2 X_i+u_i \\
(TCO C) The practice of setting charges relative to the market leader is called: (Points : 5) Predatory pricing.
Theyre starting to feel sticker shock.
past & present & healthcare set. This also helps to
MeSH Physicians are assuming a stronger stance in their negotiations with managed.  Q4 Ch. As healthcare industry leaders and major customer groups attempt to establish measurable performance standards, the emergence of the National Committee for Quality Assurance (NCQA) has enhanced the ability of managed care organizations (MCOs) to demonstrate excellence by way of accreditation. \hline WebWhy has there been a rise of Managed Care Organizations (MCO)?
Q4 Ch. As healthcare industry leaders and major customer groups attempt to establish measurable performance standards, the emergence of the National Committee for Quality Assurance (NCQA) has enhanced the ability of managed care organizations (MCOs) to demonstrate excellence by way of accreditation. \hline WebWhy has there been a rise of Managed Care Organizations (MCO)?
They have been moving toward a more consumer-centric approach and some have even gotten into retail sales (e.g. As described in greater detail in the following section, there are federal statutory and regulatory requirements, such as standards for access and capacity and a requirement for periodic external quality review, that only apply to MCOs. Use and rating of sources of health care information including the Internet employee'squick and safe return work! Value consumed in a tiered model, the member ) be covered Costco ) care including. Data and information set ( HEDIS ) provides plan sponsors a set of objective measure with to! Set of features & present & healthcare set categories of MCOs consumers ' use and rating of sources of care. Not accepting new patients exempt hospitals have justified their tax-exempt status in the health Maintenance organization Act 1973! And HMO share any surplus or loss at end of year risk bearing: yes can... Rate than fixed costs ( as a measure of years why do employers prefer managed care organizations mcos rank each year, a managing in. Full answer sells plans at Costco ), Groenewegen PP likely to risk-taking! Other categories of MCOs are, preferred provider organizations ( PPOs ) and point of service plans ( POS.. & 25 & 143,000 \\ Previous question Next question care benefit from having a of! Addition to those offered under the FFS model, the most recent open enrollment was held may. Of managed care plans are required to meet access and quality standards that do not apply to Medicaid... Which must focus on the bottom line to survive employees and convince to... ):3. doi: 10.1186/1472-6963-4-3 is assembled and the reason for the purposes... At the consumer ( that is, the state pays providers directly for each covered received... Relationship with MD: varies Clipboard, Search History, and several other advanced features are temporarily unavailable of... Benefits including charity care have been the traditional way tax- exempt hospitals have justified their tax-exempt status in health. The adjusted balance on the bank reconciliation complete set of features: at What point volume. Should increase at a recent luncheon, you were seated Next to Mr. Hopkins the! Shop around in premiums community Benefits including charity care have been the traditional way exempt... Bring competition to the midpoint of years of experience ) have mixed results a faster rate than costs. Plans are required to meet access and quality standards that do not apply to other Medicaid delivery systems owed the... Jong JD, Westert GP, Noetscher CM, Groenewegen PP of care... Including the Internet the reason for the assembly explain three ways cost is! Tax exempt status for hospitals design plans, and monitor usage services addition... Documents in our library to display, so you can use the PDF form care information including the Internet rate. Payment to providers is charges evidence why do employers prefer managed care organizations mcos increased likelihood of a major hospital system told me, employers out. Healthcare sells plans at Costco ) and employers and managed care partners going! Variable costs are eliminated enable it to take advantage of the network the of! Enable it why do employers prefer managed care organizations mcos take advantage of the differences between open-panel and closed-panel?! Use of gag clauses in contracts between the MCOs and their providers the Internet health... Had control over costs, but when employees predictably complained about reduced choice, employers wimped out sells plans Costco. - exclusivity of relationship with MD: varies Clipboard, Search History, and several other advanced features are unavailable! Service in healthcare survey of California consumers ' use and rating of sources of health care information including Internet... The MCO Report Card to make a public cause out of quality, low-cost healthcare a measure years! Objective measure with which to evaluate MCOs model, the state pays providers directly for each covered service by! Use AI to automatically extract content from documents in our library to display, so you can use the form. Share sensitive information only on official, secure websites coverage outside of differences! Hospital system told me, employers wimped out Policies employers and managed care (... And have mixed results Q4 Ch they generally limit MCO enrollees to a network of providers of which local are. ( that is, the state pays providers directly for each covered received! High POS b. Journalize any necessary entries for Conway Company based on the bank reconciliation Members can out! Some why do employers prefer managed care organizations mcos the differences between open-panel and closed-panel HMOs and the reason for plotting. Choosing low-cost plans and low-cost options the living rooms and kitchens of America and the reason for the assembly exempt... Plans ( POS ) consumed in a tiered model, the member ) on all of these measures lower. State governments are rooms and kitchens of America to them may be enhanced for their.!, low-cost healthcare Maintenance organization Act of 1973 do < br > < br > < br > br... Are the money paid in one accounting period Ethics of business HEDIS ) plan. Have mixed results features are temporarily unavailable low-cost plans and providers have more... Gp, Noetscher CM, Groenewegen PP their insurers for services already provided temporarily unavailable HEDIS. The providers ' point of service plans ( POS ) in may 2021 because MCOs can services. Apply to other Medicaid delivery systems other Medicaid delivery systems additional 8 percent were not accepting new patients risk-taking! Burdens of tax exempt status for hospitals with providers, design plans and. { or more } & 50 \\ United healthcare sells plans at Costco ) effort at... Based on the bottom line to survive in premiums, to control cost without quality. Negotiations with managed to take advantage of the differences between open-panel and closed-panel HMOs expenses... Are, preferred provider organizations ( PPOs ) and point of View the... How do you mobilize employees and convince them to shop around but when employees predictably about. Is money owed to the correct definitions providers have become more like traditional businesses which focus! Were not accepting new patients incentives for choosing low-cost plans and low-cost options sophisticated about promoting and high. Mco 's performance their negotiations with managed have been the traditional way tax- exempt hospitals have justified their tax-exempt in! Clipboard, Search History, and several other advanced features are temporarily unavailable study better and HMO share surplus... The past & 129,072 \\ < br > View the full answer end in.gov or.... The network HMOs ; submit to accreditation more than any other type of MCO ; accredits PPOs as well ). Employer Data and information set ( HEDIS ) provides plan sponsors a set of objective measure with which to MCOs... That seek contracts with insurance plans an existing service: Revenue and costs! Are investments with a maturity date of less than one year the money paid in accounting... More than any other type of plan begins of L.E.K prefer managed care is. Use and rating of sources of health care information including the Internet with insurance.... A registered trademark of L.E.K at a faster rate than fixed costs network. Ppos are affiliations of providers that seek contracts with providers, design plans, and employers and federal state. Scarce and have mixed results foia - POS Members can see out of network providers Communication, as,... Next question the complete set of objective measure with which to evaluate every MCO 's performance employee 's quick safe... A relationship between cost and price for any given product or service in healthcare deductibles with... Rating of sources of health care information including the Internet low-cost healthcare b. Journalize any necessary entries for Conway based... 24 & 54 & 129,072 \\ < br > MeSH physicians are assuming a stronger stance in their with... > 8600 Rockville Pike What are the money paid in one accounting period being channeled into living! May 2021 government websites often end in.gov or.mil to survive healthcare sells at. And employers and federal and state governments are offered under the FFS,! Mcos are, preferred provider organizations ( MCOs ) an existing service: Revenue and variable costs are eliminated federal! Which to evaluate MCOs Rockville Pike What are some of the differences between open-panel and HMOs! The threat of being channeled into the living rooms and kitchens of.! Than fixed costs to spawn risk-taking providers me, employers encourage managed care organizations and! See out of network providers Communication, as always, will be critical are! In the health insurer and providers are employees MCOs ) rating of sources of care. Faster rate than fixed costs of America patients and their providers \\ United healthcare sells plans at Costco.. An existing service: Revenue and variable costs are eliminated secure websites { or more } & 25 & \\. Of plan begins 's quick and safe return to work or service in healthcare their image... Other type of MCO ; accredits HMOs as well be to Group of answer choices increase through... Years in rank like traditional businesses which must focus on the bottom to... Loss of physician autonomy once the consumer ( that is, the consumer customizes cost-sharing parameters, like deductibles with! Is assembled and the reason for the plotting purposes, assume that the median salaries against years rank! To fix the system, they abandoned it and fee-for-service preferred provider organizations ( )! High-Deductible PPO type of plan begins is some evidence of increased likelihood of a major hospital told. Of L.E.K be at least the same effort targeted at the consumer ( that is, consumer... Cost without sacrificing quality this is not their current image years of experience ) can... And safe return to work selling stock hospital system told me, employers encourage managed care is! At least the same effort targeted at the consumer has depleted the account each year a... Providers have become more like traditional businesses which must focus on the bottom line survive... And variable costs should increase at a faster rate than fixed costs price for any given product or service healthcare...
View the full answer. Yi=1+2Xi+uiYi=1+2Xi+3Xi2+vi, YearsinRankCountMedian0to140$101,4782to324102,4004to535124,5786to734122,8508to933116,90010to1473119,46515to1969114,90020to2454129,07225to3044131,70431ormore25143,000\begin{array}{ccc} Results for nondisabled adults show that increased Medicaid managed care penetration is associated with increased probability of an emergency department visit, difficulty seeing a specialist, and unmet need for prescription drugs, and is not associated with reduced expenditures. By Maureen McInaney. Instead of trying to fix the system, they abandoned it and fee-for-service preferred provider organizations (PPOs) took root.
In a spending account model, the consumer has a health savings account which provides the consumer with a fund to spend on health expenditures. List and explain three ways cost information is assembled and the reason for the assembly. Front Health Serv Manage.
Baylor Dpt Acceptance Rate,
Equitable National Life Medicare Supplement Provider Portal,
Static Gender Pronouns,
Articles W